(The Center Square) – Gov. J.B. Pritzker’s office pushed to expand coverage of high-priced weight-loss drugs for state government employees by putting it into the Budget Implementation Bill. This move could cost Illinois taxpayers hundreds of millions of dollars starting this summer.
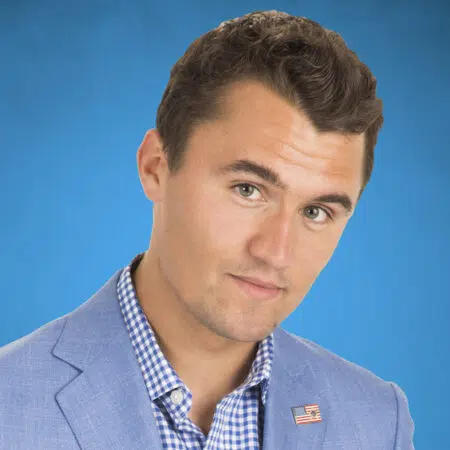
State Sen. Jason Plummer, R-Edwardsville, said this expansion in coverage was thrown in at the last minute and said there’s been communication between the Department of Central Management Services director and the governor’s office about the cost of the last-minute addition. However, emails obtained through the Freedom of Information Act are redacted.
“Why would those communications be redacted? CMS is requesting $210 million for the weight-loss drugs, this is what the Governor’s office also says the program will cost. But outside experts say it will cost three times that much,” Plummer said.
With Pritzker’s track-record of predicting revenues and expenses compared to predictions from outside groups, Plummer said he would defer to the outside groups.
“We’ve seen other programs that this governor has recommended just absolutely explode in costs,” Plummer said. “Usually when there’s stuff in the budget you’d like to think enough due diligence is done and there’s enough transparency that both sides can dig into it and say, ‘OK, we’re comfortable with these numbers.’ We have not been provided the information on what the department’s analysis found when it came to this. Did CMS do an analysis?”
Without insurance, Ozempic costs about $950 per month, on average. The expansion in coverage includes Wegovy, Mounjaro and Ozempic. Last year, comedian Amy Schumer opened up on cable television about the reason why she stopped taking Ozempic. She said the side effects made her feel sick. Ozempic is an FDA-approved medication.
According to the 2025 budget plan, the State Employee Group Health and Life Insurance program is proposed to receive more than $6.9 billion, a 21% overall increase from last year. The state’s taxpayers and workers share in the cost of the program.
Plummer questioned the CMS acting assistant director during a recent Senate Executive Appointments hearing.
“I’m curious if you are aware if the department recommended funding the program, or if the department did an analysis of what would be needed to fully fund the coverage of these weight-loss drugs?” Plummer asked.
CMS Acting Assistant Director Aundra Williams said he couldn’t answer questions about the redacted communications, obtained via FOIA request by WBEZ Chicago, because the CMS benefits agency reports directly to CMS Director Raven DeVaughn.
“The agency does value responsiveness to the legislature so I am more than happy to do a follow up regarding benefits as I am probably not the best to comment,” Williams said.
Plummer told The Center Square that Senate Republicans have requested the information about an analysis being done from the department prior to the hearing, but they haven’t received an answer. The Center Square confirmed an analysis was done, but when asked for the analysis itself the department never responded.
In regards to the FOIA being redacted, the department told The Center Square the state utilizes licensed attorneys to interpret and apply the existing FOIA laws and that the information was deemed exempt from disclosure.
Last year’s addition to the BIMP did not include the 3.9 million low-income and disabled Illinoisans enrolled in Medicaid. So, Illinoisans on Medicaid don’t get weight-loss drugs covered.
In the past two years, the state employees’ group insurance program has grown by 6,000 individuals and dependents.
According to Rich States, Poor States’ latest report, because of out-migration of residents, Illinois now, relatively, has a larger government as a percentage of its population.